A nurse is preparing to administer lactated ringer’s 2 l – A nurse is preparing to administer lactated ringer’s 2L – a common procedure in healthcare settings. This involves a meticulous process of preparing and administering the solution, ensuring patient safety and monitoring their response. The decision to administer lactated ringer’s is based on a thorough assessment of the patient’s condition, considering factors like fluid volume status, electrolyte imbalances, and overall health.
Lactated Ringer’s solution is a versatile intravenous fluid commonly used to replenish fluids and electrolytes in patients experiencing dehydration, blood loss, or electrolyte imbalances. It closely resembles the composition of human plasma, making it a suitable choice for various clinical scenarios. This article will delve into the intricacies of preparing and administering lactated ringer’s solution, exploring the rationale behind its use, potential complications, and essential nursing considerations.
Lactated Ringer’s Solution
Lactated Ringer’s solution is a balanced electrolyte solution commonly used in intravenous fluid therapy. It is a crystalloid solution, meaning it contains electrolytes and other small molecules that can easily move across cell membranes. It is designed to mimic the electrolyte composition of the body’s extracellular fluid, making it a suitable replacement for lost fluids and electrolytes.
Composition and Physiological Rationale
Lactated Ringer’s solution is composed of:
- Sodium (Na+): 130 mEq/L
- Potassium (K+): 4 mEq/L
- Calcium (Ca2+): 3 mEq/L
- Chloride (Cl-): 109 mEq/L
- Lactate (C3H5O3-): 28 mEq/L
The physiological rationale behind this composition is to provide a balanced electrolyte solution that can:
- Replace lost fluids and electrolytes: This is particularly important in cases of dehydration, hypovolemia, and electrolyte imbalances.
- Maintain intravascular volume: By providing fluids and electrolytes, Lactated Ringer’s solution helps to expand blood volume and maintain blood pressure.
- Correct metabolic acidosis: Lactate is a buffer that can help to neutralize excess hydrogen ions (H+) in the blood, which can occur in conditions like shock and sepsis.
Indications for Administration
Lactated Ringer’s solution is commonly used in various clinical settings, including:
- Hypovolemia: It is used to treat fluid volume depletion due to conditions such as dehydration, blood loss, and burns.
- Electrolyte imbalances: It can be used to correct imbalances in sodium, potassium, and calcium levels.
- Metabolic acidosis: It can help to buffer excess hydrogen ions in the blood, which can occur in conditions like shock and sepsis.
- Surgery: It is often used to replace fluids lost during surgery and to maintain hemodynamic stability.
- Trauma: It is a mainstay fluid for the management of trauma patients, particularly in cases of hypovolemic shock.
Comparison with Other Intravenous Fluids
Lactated Ringer’s solution is often compared to other intravenous fluids, such as Normal Saline (0.9% NaCl) and D5W (5% dextrose in water). Here’s a comparison:
| Fluid | Composition | Indications | Advantages | Disadvantages |
|---|---|---|---|---|
| Lactated Ringer’s | Balanced electrolyte solution | Hypovolemia, electrolyte imbalances, metabolic acidosis | More physiological than Normal Saline, can help correct metabolic acidosis | May not be suitable for patients with liver disease or renal failure |
| Normal Saline | 0.9% NaCl | Hypovolemia, electrolyte imbalances | Simple and readily available | Can lead to hyperchloremia and metabolic acidosis |
| D5W | 5% dextrose in water | Fluid replacement, calorie provision | Provides calories, can help correct hypoglycemia | Can lead to fluid overload and hyponatremia |
Administration of Lactated Ringer’s
Administering Lactated Ringer’s solution requires meticulous preparation and careful execution to ensure patient safety and efficacy. This section will detail the steps involved in preparing and administering 2 liters of Lactated Ringer’s solution, explore different routes of intravenous fluid administration, and provide a comprehensive overview of the necessary equipment and supplies.
Routes of Administration for Intravenous Fluids
Intravenous fluid administration is a common practice in healthcare, providing a direct and efficient route for delivering fluids, electrolytes, and medications into the bloodstream. Different routes of administration exist, each with unique advantages and disadvantages.
- Peripheral Intravenous (IV) Access: This is the most common route, involving insertion of a catheter into a peripheral vein, typically in the arm or hand. It offers convenience and is suitable for most intravenous fluid administrations. However, it may be challenging to maintain long-term IV access in certain individuals, particularly those with poor peripheral vein access or those requiring frequent IV therapy.
- Central Venous Access: This route involves inserting a catheter into a large central vein, such as the superior vena cava or internal jugular vein. It offers a larger vein diameter, allowing for higher fluid flow rates and prolonged IV access. This route is preferred for administering hypertonic solutions, medications that can irritate peripheral veins, or for long-term IV therapy. However, central venous access carries a higher risk of complications, including pneumothorax, hemothorax, and air embolism.
- Intraosseous Access: This route involves inserting a needle into the bone marrow, providing direct access to the systemic circulation. It is a valuable option for emergency situations when peripheral or central venous access is not feasible, such as in cases of shock or cardiac arrest. However, it is a painful procedure and carries a risk of infection and bone marrow damage.
Equipment and Supplies
Administering Lactated Ringer’s solution requires a specific set of equipment and supplies to ensure a safe and sterile procedure.
- Intravenous Fluid Bag: A 2-liter bag of Lactated Ringer’s solution, pre-filled and sterile, is essential for administering the required volume.
- Intravenous Administration Set: This sterile set includes a tubing with a drip chamber, a roller clamp for flow rate regulation, and a spike for attaching to the fluid bag. It ensures safe and controlled delivery of the fluid.
- Intravenous Catheter: A suitable intravenous catheter, typically 18 gauge or larger, is required for peripheral or central venous access. The size of the catheter is chosen based on the patient’s condition and the intended flow rate.
- Sterile Gloves: Wearing sterile gloves ensures proper asepsis and minimizes the risk of contamination during the procedure.
- Sterile Gauze Pads: Sterile gauze pads are used for cleaning the insertion site and securing the catheter.
- Alcohol Swabs: Alcohol swabs are used for disinfecting the insertion site before catheter insertion.
- Tourniquet: A tourniquet is used to temporarily constrict blood flow to the insertion site, making the vein more prominent and easier to access.
- Syringe: A syringe is used to flush the catheter with saline solution after insertion, ensuring patency and minimizing the risk of clotting.
- Safety Needle: A safety needle is used for drawing up saline solution for flushing the catheter. It reduces the risk of needlestick injuries.
- Tape or Securement Device: Tape or a securement device is used to secure the catheter to the patient’s skin, preventing accidental dislodgement.
Preparation and Administration, A nurse is preparing to administer lactated ringer’s 2 l
Preparing and administering Lactated Ringer’s solution involves a series of steps designed to ensure patient safety and effectiveness.
- Gather Equipment and Supplies: Assemble all necessary equipment and supplies, ensuring they are sterile and ready for use.
- Prepare the Infusion Site: Choose a suitable insertion site, typically a peripheral vein in the arm or hand. Clean the site with alcohol swabs and apply a tourniquet to make the vein more prominent.
- Insert the Intravenous Catheter: Insert the intravenous catheter into the chosen vein, using aseptic technique to minimize the risk of infection.
- Secure the Catheter: Secure the catheter to the patient’s skin using tape or a securement device. Ensure the catheter is secure and comfortable for the patient.
- Flush the Catheter: Flush the catheter with saline solution using a syringe to ensure patency and minimize the risk of clotting.
- Connect the IV Fluid Bag: Connect the IV fluid bag to the intravenous administration set, ensuring the spike is securely attached to the bag port.
- Regulate the Flow Rate: Adjust the roller clamp on the administration set to achieve the desired flow rate. The flow rate is determined by the patient’s condition and the volume of fluid to be administered.
- Monitor the Infusion: Monitor the infusion site regularly for signs of infiltration, extravasation, or phlebitis. Also, monitor the patient’s vital signs, including blood pressure, heart rate, and urine output, to assess fluid balance and response to the infusion.
- Document the Infusion: Document the type and volume of fluid administered, the infusion site, the flow rate, and any adverse events encountered. This documentation is essential for tracking patient care and ensuring continuity of care.
Patient Assessment and Monitoring
Administering large volumes of intravenous fluids, such as Lactated Ringer’s solution, requires careful monitoring to ensure patient safety and prevent potential complications. It is essential to assess the patient’s condition before, during, and after fluid administration.
Vital Signs and Clinical Parameters
Monitoring vital signs and clinical parameters is crucial to detect any adverse effects of fluid administration. The following parameters should be monitored:
- Before administration:
- Baseline vital signs, including temperature, pulse, respiratory rate, blood pressure, and oxygen saturation.
- Assessment of hydration status, including skin turgor, mucous membrane moisture, and urine output.
- Electrolyte levels, especially sodium, potassium, and chloride.
- Renal function, as indicated by creatinine and blood urea nitrogen (BUN) levels.
- Cardiac function, as indicated by electrocardiogram (ECG) and echocardiogram.
- During administration:
- Frequent monitoring of vital signs, particularly blood pressure and heart rate.
- Assessment of fluid balance, including intake and output.
- Monitoring for signs of fluid overload, such as edema, dyspnea, crackles in the lungs, and increased jugular venous distention.
- Monitoring for signs of electrolyte imbalances, such as muscle weakness, fatigue, and arrhythmias.
- After administration:
- Continue monitoring vital signs and fluid balance.
- Assess for any signs of complications, such as pulmonary edema, heart failure, or electrolyte disturbances.
- Monitor for improvement in the patient’s clinical condition.
Potential Complications of Large Volume Fluid Administration
Administering large volumes of intravenous fluids can lead to several potential complications, including:
- Fluid overload: This occurs when the body receives more fluids than it can handle, leading to increased blood volume, elevated blood pressure, and potentially pulmonary edema.
- Electrolyte imbalances: Intravenous fluids can alter electrolyte levels, particularly sodium, potassium, and chloride. This can lead to various complications, including arrhythmias, muscle weakness, and seizures.
- Pulmonary edema: This occurs when excess fluid accumulates in the lungs, making breathing difficult.
It can be a serious complication of fluid overload.
- Heart failure: In patients with pre-existing heart conditions, large volumes of fluids can overload the heart, leading to heart failure.
- Increased intracranial pressure: In patients with head injuries or other conditions affecting the brain, rapid fluid administration can increase intracranial pressure, potentially leading to neurological complications.
Monitoring Plan and Interventions
To minimize the risk of complications, a comprehensive monitoring plan should be implemented. This plan should include:
- Frequent vital sign monitoring: Blood pressure, heart rate, respiratory rate, and oxygen saturation should be monitored frequently, especially during the initial stages of fluid administration.
- Fluid balance monitoring: Accurate records of fluid intake and output should be maintained to assess the patient’s fluid status.
- Electrolyte monitoring: Serum electrolyte levels, particularly sodium, potassium, and chloride, should be monitored regularly, especially in patients at risk for electrolyte imbalances.
- Cardiac monitoring: Continuous ECG monitoring may be necessary in patients with pre-existing cardiac conditions or those at risk for cardiac complications.
- Pulmonary assessment: Auscultation of the lungs for crackles or wheezes should be performed regularly to detect early signs of pulmonary edema.
- Neurological assessment: Assess for changes in mental status, such as confusion, lethargy, or seizures, which may indicate increased intracranial pressure.
Nursing Considerations
The administration of Lactated Ringer’s solution requires meticulous attention to detail and a comprehensive understanding of the patient’s individual needs. Nurses play a crucial role in ensuring the safe and effective delivery of this fluid therapy, encompassing patient assessment, monitoring, and education.
Key Nursing Responsibilities
Nurses bear significant responsibility for the safe and effective administration of Lactated Ringer’s solution. This includes:
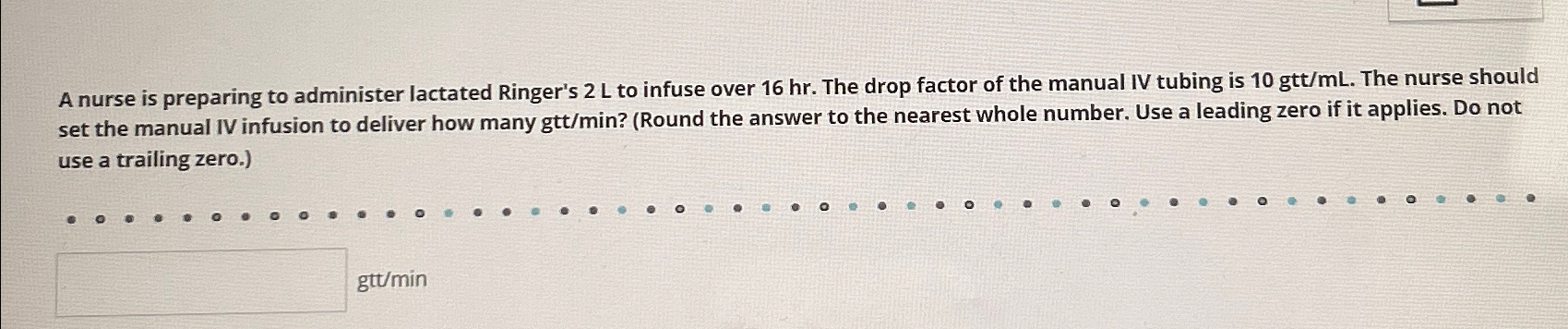
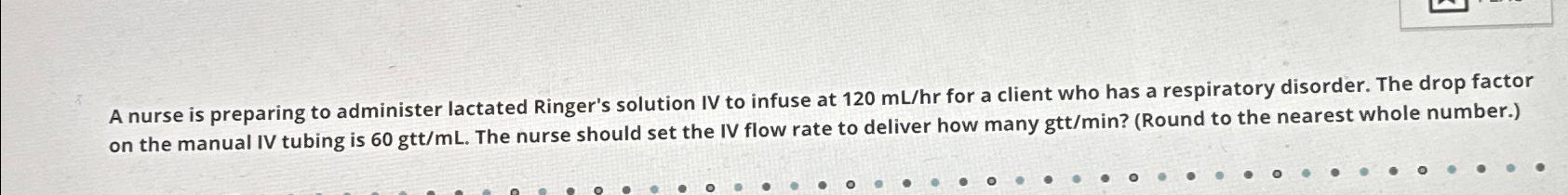
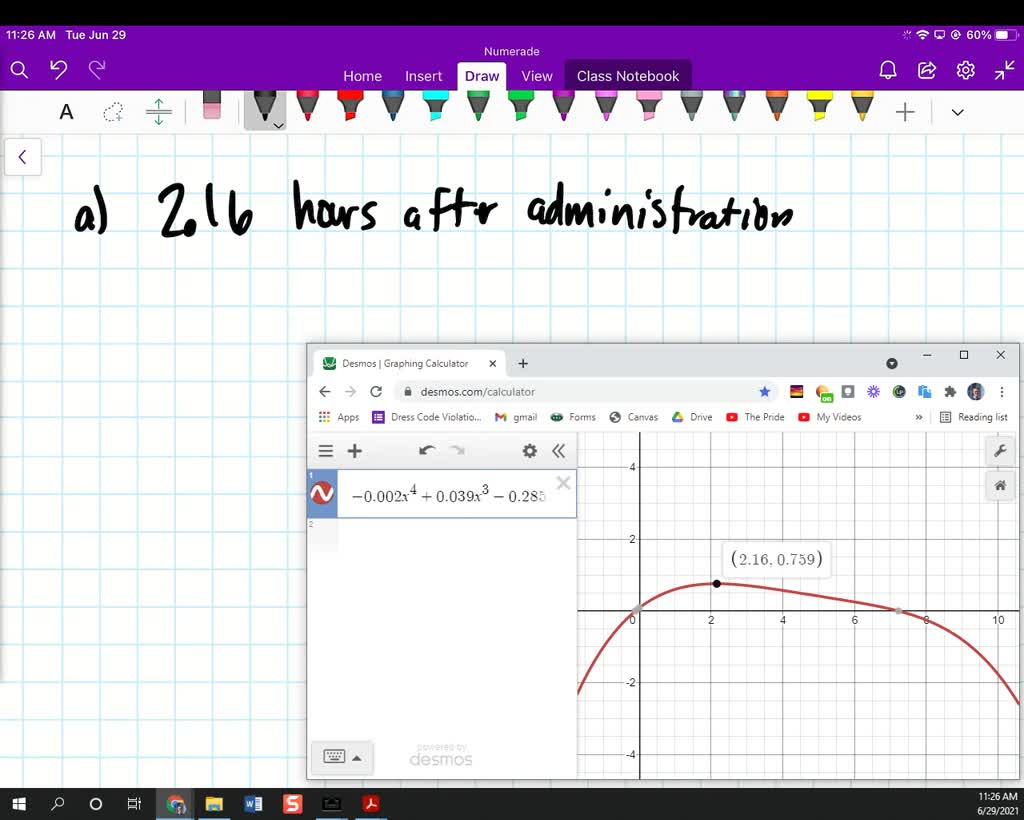
- Accurate Dosage and Rate Calculation: Nurses must carefully calculate the appropriate dosage and rate of administration based on the patient’s individual needs and the physician’s orders. This involves considering factors such as weight, age, and clinical condition.
- Route of Administration: Nurses must select the appropriate route of administration, whether intravenous (IV) or subcutaneous, based on the patient’s condition and the physician’s orders. IV administration is typically preferred for rapid fluid replacement, while subcutaneous administration is often used for long-term hydration.
- Site Selection and Insertion: When administering Lactated Ringer’s solution intravenously, nurses must carefully select the appropriate IV site, ensuring proper vein selection and aseptic technique to minimize the risk of complications such as phlebitis or infiltration. The site should be regularly monitored for signs of inflammation, redness, or swelling.
- Fluid Balance Monitoring: Nurses must diligently monitor the patient’s fluid balance, including intake and output, to ensure adequate hydration and prevent fluid overload. This involves recording fluid intake from all sources, including oral fluids, IV fluids, and medications, as well as measuring urine output and any other fluid losses, such as drainage from wounds or vomitus.
- Vital Sign Monitoring: Regular monitoring of vital signs, including temperature, pulse, blood pressure, and respiratory rate, is essential to detect any adverse effects of fluid therapy. Changes in vital signs can indicate fluid overload, electrolyte imbalances, or other complications. Nurses must be vigilant in observing these changes and reporting them to the physician promptly.
- Patient Assessment and Monitoring: Nurses must continuously assess the patient’s condition and monitor for any signs or symptoms of complications, such as edema, shortness of breath, or changes in mental status. They should also assess the patient’s response to the fluid therapy and make adjustments to the rate of administration as needed.
Patient Education and Communication
Effective communication with the patient is crucial for ensuring their understanding of the purpose and potential side effects of fluid therapy. Nurses should explain the rationale for administering Lactated Ringer’s solution, emphasizing its role in restoring fluid balance and maintaining vital functions. It is essential to inform the patient about potential side effects, such as fluid overload, electrolyte imbalances, and allergic reactions, and to encourage them to report any unusual symptoms promptly.
- Explanation of Purpose: Nurses should explain the purpose of Lactated Ringer’s solution in simple, understandable terms. For example, they might say, “This fluid will help to replace the fluids you’ve lost and keep your body hydrated.”
- Potential Side Effects: Nurses should discuss the potential side effects of Lactated Ringer’s solution, including fluid overload, electrolyte imbalances, and allergic reactions. They should also provide clear instructions on how to report any unusual symptoms promptly. For example, they might say, “Some people experience side effects from this fluid, such as swelling in the legs or feet, shortness of breath, or a rash.
If you notice any of these symptoms, please let us know right away.”
- Monitoring and Follow-Up: Nurses should emphasize the importance of monitoring the patient’s response to the fluid therapy and following up with the physician as needed. They should also provide clear instructions on how to contact the physician or nurse if the patient has any questions or concerns. For example, they might say, “We’ll be monitoring your progress closely, and you’ll be able to contact us anytime if you have any questions or concerns.”
Essential Nursing Interventions
To ensure safe and effective administration of Lactated Ringer’s solution, nurses must implement a comprehensive set of interventions. These interventions encompass patient assessment, monitoring, and medication administration, and are designed to minimize the risk of complications and optimize patient outcomes.
- Verify Physician’s Orders: Before administering any medication or fluid, nurses must carefully verify the physician’s orders. This includes checking the medication name, dosage, route of administration, and frequency. Nurses should also verify any allergies or contraindications.
- Patient Assessment: Prior to administering Lactated Ringer’s solution, nurses must conduct a thorough patient assessment, including vital signs, fluid balance, and any relevant medical history. This assessment helps to identify any potential risks or contraindications.
- IV Site Selection and Insertion: When administering Lactated Ringer’s solution intravenously, nurses must carefully select the appropriate IV site, ensuring proper vein selection and aseptic technique. They should also monitor the IV site regularly for signs of inflammation, redness, or swelling.
- Fluid Balance Monitoring: Nurses must diligently monitor the patient’s fluid balance, including intake and output, to ensure adequate hydration and prevent fluid overload. This involves recording fluid intake from all sources, including oral fluids, IV fluids, and medications, as well as measuring urine output and any other fluid losses.
- Vital Sign Monitoring: Regular monitoring of vital signs, including temperature, pulse, blood pressure, and respiratory rate, is essential to detect any adverse effects of fluid therapy. Changes in vital signs can indicate fluid overload, electrolyte imbalances, or other complications. Nurses must be vigilant in observing these changes and reporting them to the physician promptly.
- Patient Education and Communication: Nurses should provide clear and concise information to the patient about the purpose, potential side effects, and monitoring of Lactated Ringer’s solution. They should also encourage the patient to report any unusual symptoms promptly.
- Documentation: Nurses must accurately document all aspects of the administration of Lactated Ringer’s solution, including the date and time of administration, the dosage, the route of administration, and any patient responses or complications. This documentation is essential for ensuring continuity of care and for legal purposes.
Administering lactated ringer’s solution is a crucial aspect of nursing practice, requiring careful attention to detail, meticulous monitoring, and a thorough understanding of patient needs. By following established protocols, nurses can ensure the safe and effective administration of this vital fluid, contributing to the well-being and recovery of their patients. This process underscores the importance of nurses’ role in patient care, emphasizing their dedication to delivering compassionate and evidence-based care.
Question & Answer Hub: A Nurse Is Preparing To Administer Lactated Ringer’s 2 L
What are the potential side effects of administering lactated ringer’s solution?
Potential side effects include fluid overload, electrolyte imbalances, and allergic reactions. These are usually manageable with careful monitoring and adjustments to the infusion rate.
How long does it typically take to administer 2 liters of lactated ringer’s?
The infusion time varies depending on the patient’s needs and the rate set by the healthcare provider. It can range from a few hours to several hours.
Can lactated ringer’s be administered to all patients?
No, lactated ringer’s may not be suitable for all patients. Certain medical conditions, such as heart failure or kidney disease, may necessitate alternative fluids.