Can you bike with plantar fasciitis? This question often arises for individuals struggling with this common foot condition. Plantar fasciitis, characterized by pain in the heel and arch of the foot, can significantly impact daily activities, including biking. While it may seem daunting, with proper understanding and strategies, biking with plantar fasciitis is possible. This journey will explore the challenges and solutions, empowering you to enjoy cycling while managing your condition.
Plantar fasciitis occurs when the thick band of tissue on the bottom of your foot, called the plantar fascia, becomes inflamed. This inflammation can be caused by overuse, improper footwear, tight calf muscles, or even obesity. The pain often worsens after rest or in the morning, and it may feel better after some activity. For those who love biking, the thought of having to give it up can be disheartening.
However, with the right approach, you can continue to enjoy cycling while managing your plantar fasciitis.
Understanding Plantar Fasciitis
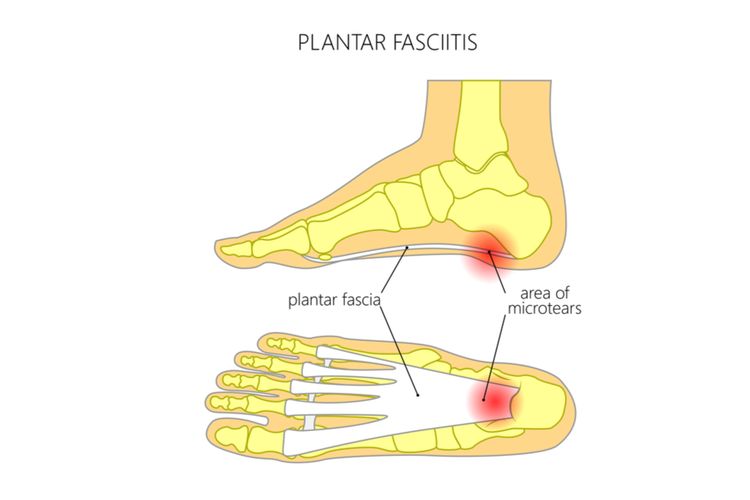
Plantar fasciitis is a common condition that causes pain in the heel and arch of the foot. It occurs when the plantar fascia, a thick band of tissue that runs along the bottom of the foot, becomes inflamed. This inflammation can be caused by a variety of factors, including overuse, improper footwear, and tight calf muscles.
Causes of Plantar Fasciitis
Plantar fasciitis can be caused by a number of factors, including:
- Overuse: Engaging in activities that put repeated stress on the plantar fascia, such as running, jumping, or standing for long periods, can lead to inflammation.
- Improper footwear: Wearing shoes that lack proper support or cushioning can put excessive strain on the plantar fascia. This includes high heels, flat shoes, and shoes that are worn out.
- Tight calf muscles: Tight calf muscles can pull on the plantar fascia, increasing tension and inflammation.
- Obesity: Excess weight puts extra stress on the plantar fascia, making it more susceptible to inflammation.
- Age: Plantar fasciitis is more common in people over 40, as the plantar fascia can become less flexible with age.
- Certain medical conditions: Conditions like diabetes, arthritis, and flat feet can increase the risk of developing plantar fasciitis.
Symptoms of Plantar Fasciitis
The most common symptom of plantar fasciitis is pain in the heel that is worse in the morning or after a period of rest. The pain may also be worse after exercise or standing for long periods. Other symptoms can include:
- Stiffness in the heel
- Tenderness along the bottom of the heel
- Pain that radiates into the arch of the foot
- Pain that is worse when you press on the bottom of the heel
Impact of Plantar Fasciitis on Daily Activities
Plantar fasciitis can significantly impact daily activities, including biking. The pain and stiffness caused by the condition can make it difficult to pedal efficiently and comfortably. It can also make it challenging to walk, stand, and participate in other activities that involve putting weight on the feet.
Biking with Plantar Fasciitis
While cycling can be a great low-impact exercise, it’s important to understand the potential challenges and how to adapt your biking experience if you have plantar fasciitis.
Potential Challenges of Biking with Plantar Fasciitis
Plantar fasciitis can make biking uncomfortable and even painful. The repetitive motion of pedaling can aggravate the condition, especially if your bike isn’t properly fitted or if you’re not wearing supportive footwear.
- Increased Pain and Inflammation: The constant pressure and stretching of the plantar fascia during pedaling can worsen pain and inflammation.
- Limited Range of Motion: Pain and stiffness in the foot can limit your ability to comfortably move your foot through the full range of motion required for efficient pedaling.
- Increased Risk of Injury: If you’re not properly supporting your foot and ankle, you may be at increased risk of developing other injuries, such as shin splints or Achilles tendonitis.
Importance of Proper Bike Fit and Adjustments for Plantar Fasciitis, Can you bike with plantar fasciitis
A properly fitted bike is crucial for comfortable and efficient cycling, especially with plantar fasciitis. A bike fit specialist can help adjust your bike to minimize stress on your feet and ankles.
- Seat Height: The correct seat height ensures that your knees are slightly bent at the bottom of the pedal stroke, reducing strain on your feet and ankles.
- Cleat Position: Adjusting the position of your cleats, which attach your shoes to the pedals, can help align your feet and reduce pressure on the plantar fascia.
- Handlebar Height: Adjusting the handlebar height can help improve your posture and reduce stress on your lower body.
Role of Supportive Footwear and Insoles
Choosing the right shoes and insoles is essential for managing plantar fasciitis while biking.
- Supportive Cycling Shoes: Look for shoes with good arch support, a firm heel counter, and a wide toe box to accommodate the natural shape of your foot.
- Custom Orthotics: Custom orthotics can provide personalized support and cushioning for your feet, reducing stress on the plantar fascia. These are often recommended by podiatrists or physical therapists.
- Over-the-Counter Insoles: If custom orthotics aren’t an option, consider over-the-counter insoles designed for arch support and cushioning.
Biking Techniques and Strategies: Can You Bike With Plantar Fasciitis

Cycling with plantar fasciitis requires careful consideration of techniques and strategies to minimize strain on the plantar fascia. By implementing these methods, you can enjoy biking while promoting healing and preventing further injury.
Adjusting Bike Fit
Proper bike fit is crucial for reducing stress on the plantar fascia. A well-adjusted bike ensures that your feet are positioned correctly, distributing weight evenly and minimizing pressure on the heels. Here are some key adjustments:
- Seat Height: Adjust the seat height to ensure a slight bend in your knee when the pedal is at its lowest point. This position helps distribute weight evenly and reduces strain on the plantar fascia.
- Cleats: If you use cleats, ensure they are positioned to allow for a natural foot position. Avoid excessive inward or outward rotation, which can put stress on the plantar fascia.
- Foot Position: Experiment with different foot positions on the pedals. Some cyclists find that placing their feet slightly forward on the pedal reduces pressure on the heels.
Biking Technique
Maintaining proper biking technique can significantly reduce stress on the plantar fascia. Here are some tips:
- Cadence: Aim for a higher cadence (pedal revolutions per minute), typically around 80-90 RPM. This helps reduce the amount of force applied to the plantar fascia during each pedal stroke.
- Smooth Pedaling: Avoid harsh or jerky movements when pedaling. Smooth, consistent pedaling helps minimize stress on the feet and ankles.
- Relaxed Grip: Maintain a relaxed grip on the handlebars. A tight grip can lead to tension in the arms and shoulders, which can indirectly affect the plantar fascia.
Stretching and Exercises
Regular stretching and exercises are essential for managing plantar fasciitis and promoting healing. Here are some exercises that can be beneficial:
- Calf Stretches: Calf stretches help lengthen the calf muscles, which can reduce tension on the plantar fascia.
- Plantar Fascia Stretches: These stretches directly target the plantar fascia, helping to improve flexibility and reduce tightness.
- Toe Curls: Toe curls strengthen the intrinsic muscles of the foot, which can help support the plantar fascia.
Gradual Increase in Intensity
When returning to biking after plantar fasciitis, it is crucial to gradually increase duration and intensity.
- Start Slowly: Begin with short rides and gradually increase the duration and intensity over time. This allows your body to adapt and reduces the risk of re-injury.
- Listen to Your Body: Pay attention to any pain or discomfort during your rides. If you experience pain, stop and rest. Do not push through pain.
- Rest and Recovery: Allow adequate rest and recovery time between rides. This allows your body to repair and rebuild, reducing the risk of further injury.
Considerations and Recommendations

While biking can be a great exercise option for those with plantar fasciitis, it’s crucial to approach it with caution and prioritize pain management. Remember, every individual’s experience with plantar fasciitis is unique, and what works for one person may not work for another.
Managing Pain and Discomfort
Managing pain and discomfort while biking is essential for a safe and enjoyable experience. Here are some tips:
- Start slowly and gradually increase your distance and intensity: Avoid pushing yourself too hard too soon. Listen to your body and take breaks when needed.
- Choose the right bike and adjust your seat height: A comfortable bike with a seat height that promotes proper leg extension can reduce stress on your feet.
- Wear supportive shoes: Opt for shoes with good arch support and cushioning to minimize strain on your plantar fascia.
- Use custom orthotics or insoles: These can provide additional support and cushioning, especially if you have flat feet or high arches.
- Consider compression socks: Compression socks can help improve blood circulation and reduce swelling in your feet.
- Apply ice to your feet after biking: This can help reduce inflammation and pain.
- Stretch your calf muscles and plantar fascia regularly: Stretching can help improve flexibility and reduce tightness in your feet and ankles.
- Avoid prolonged standing or walking: Minimize activities that put extra stress on your feet.
Seeking Professional Guidance
It’s crucial to consult a healthcare provider or physical therapist for personalized advice and treatment. They can:
- Diagnose your condition accurately: A healthcare professional can determine the severity of your plantar fasciitis and rule out other potential causes of your pain.
- Develop a personalized treatment plan: This may involve medication, physical therapy, orthotics, or other interventions.
- Provide guidance on safe biking practices: They can help you adjust your biking routine and technique to minimize stress on your feet.
Resources and Support Groups
There are numerous resources and support groups available for individuals with plantar fasciitis:
- American Academy of Orthopaedic Surgeons (AAOS): The AAOS provides information about plantar fasciitis, including treatment options and prevention strategies.
- American Physical Therapy Association (APTA): The APTA offers resources on physical therapy for plantar fasciitis, including exercises and stretches.
- Plantar Fasciitis Support Groups: Online forums and support groups provide a platform for sharing experiences, tips, and encouragement with others who have plantar fasciitis.
Biking with plantar fasciitis can be a rewarding experience, allowing you to stay active and enjoy the outdoors while managing your condition. By understanding the challenges, implementing appropriate strategies, and seeking professional guidance, you can navigate this journey successfully. Remember, consistency in stretching, proper footwear, and gradual increases in activity are key to achieving your goals. Embrace the power of your spirit and the beauty of cycling, and discover a path that allows you to move forward with strength and resilience.
Question Bank
Can I bike every day with plantar fasciitis?
It’s best to start gradually and listen to your body. Begin with shorter rides and gradually increase the duration and intensity as your condition improves.
What type of bike is best for plantar fasciitis?
A bike with a comfortable saddle and good suspension can help reduce stress on your feet. Consider a hybrid or comfort bike for a more upright riding position.
Are there any specific exercises for plantar fasciitis?
Yes, stretching exercises for the plantar fascia, calf muscles, and Achilles tendon are crucial. Consult with a physical therapist for personalized recommendations.
Should I wear special shoes for biking with plantar fasciitis?
Yes, supportive shoes with good arch support and cushioning are essential. Consider using orthotics or insoles to provide additional support.